ENDOCRINE DISORDERS: DIABETES MANAGEMENT AND DIABETIC KETOACIDOSIS (DKA)
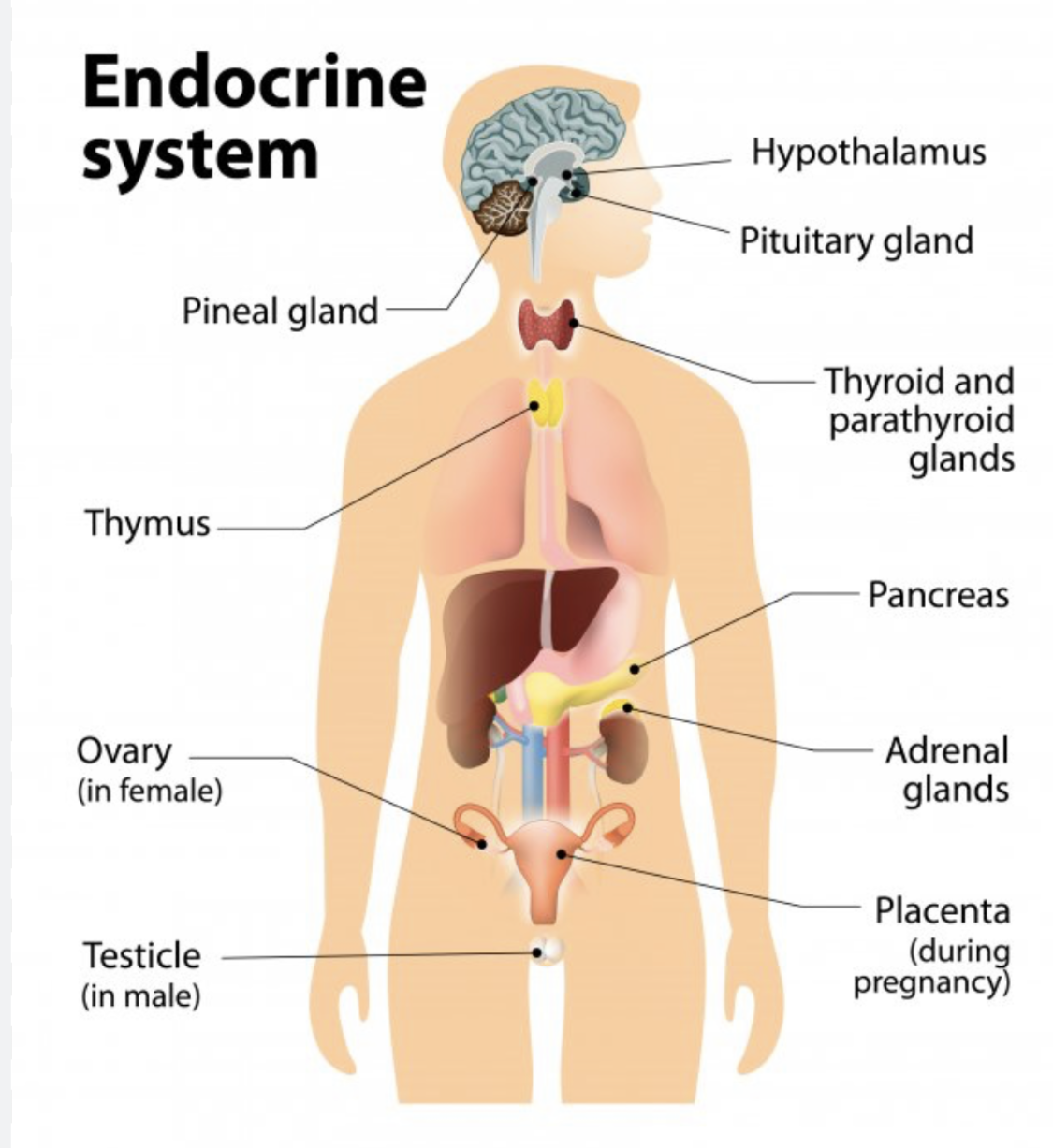
Managing endocrine disorders, particularly diabetes, is essential for ensuring that patients maintain stable blood glucose levels and prevent serious complications like diabetic ketoacidosis (DKA). Diabetes is a chronic condition where the body cannot properly process glucose due to either insufficient insulin production (type 1 diabetes) or ineffective use of insulin (type 2 diabetes). Both conditions require consistent monitoring and management to prevent hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar), with DKA being a life-threatening consequence if blood glucose is not well-controlled.
In this blog post, we will explore how nurses can effectively manage diabetes and prevent DKA, focusing on key interventions, monitoring, and patient education. Whether preparing for the NCLEX or working in clinical settings, understanding diabetes management and DKA is crucial for positive patient outcomes.
Diabetes management
Effective diabetes management is essential to prevent complications, enhance quality of life, and reduce the risk of life-threatening conditions like DKA. Nurses play a significant role in educating patients, administering medications, and monitoring for signs of imbalance.
Key interventions for diabetes management:
– Monitoring blood glucose levels regularly. Blood glucose monitoring helps detect fluctuations in glucose levels and adjust treatments accordingly. Nurses should educate patients on the importance of self-monitoring and how to use glucose meters properly.
– Administering insulin and oral hypoglycemic agents. Depending on the type of diabetes, patients may require insulin therapy or oral medications such as metformin. Nurses must ensure accurate dosing, teach patients how to administer insulin safely, and monitor for side effects like hypoglycemia.
– Promoting lifestyle modifications. Diet and exercise are vital components of diabetes management. Nurses should provide education on meal planning, carbohydrate counting, and the benefits of regular physical activity in maintaining stable blood glucose levels.
– Monitoring for complications. Diabetes can lead to long-term complications such as neuropathy, nephropathy, retinopathy, and cardiovascular issues. Nurses need to assess for early signs of these complications and collaborate with other healthcare professionals to manage them effectively.
Diabetic ketoacidosis (DKA) management
Diabetic ketoacidosis is a severe and potentially life-threatening complication of uncontrolled diabetes, primarily seen in type 1 diabetes. It occurs when there is not enough insulin in the body to use glucose for energy, leading to the breakdown of fat for fuel and the production of ketones, which causes the blood to become acidic. DKA requires prompt recognition and intervention to prevent coma or death.
Key interventions for DKA management:
– Immediate fluid replacement. DKA leads to severe dehydration due to excessive urination and vomiting. Nurses should administer intravenous (IV) fluids to restore blood volume, correct dehydration, and help lower blood glucose levels.
– Insulin therapy. Rapid-acting insulin is administered intravenously to reduce blood glucose and stop the production of ketones. Nurses must closely monitor glucose levels and adjust the insulin infusion rate as needed to prevent hypoglycemia.
– Electrolyte monitoring and replacement. DKA can cause significant imbalances in electrolytes like potassium, sodium, and bicarbonate. Nurses should monitor electrolyte levels and administer replacement therapies to maintain homeostasis.
– Monitoring for complications. Nurses must be vigilant for complications such as hypoglycemia, cerebral edema, and electrolyte imbalances during DKA treatment. Regular monitoring of vital signs, glucose levels, and neurological status is crucial.
Comprehensive diabetes and DKA care
Both diabetes and DKA require a multidisciplinary approach for optimal management and recovery. Nurses are pivotal in coordinating care, educating patients and families, and ensuring that treatment plans are followed.
– Patient education is critical for preventing DKA and managing diabetes long-term. Patients must understand the importance of medication adherence, regular glucose monitoring, and recognizing early signs of hyperglycemia and DKA. Nurses should teach patients about sick day management (how to adjust insulin and food intake when ill) to prevent DKA.
– Emotional and psychological support is essential. Diabetes is a lifelong condition, and managing it can be overwhelming for patients. Nurses should provide emotional support, connect patients with support groups, and address mental health concerns like anxiety or depression that may arise.
– Collaborating with the healthcare team is vital. Nurses must work closely with endocrinologists, dietitians, pharmacists, and other healthcare professionals to create individualized care plans that meet the unique needs of each patient.
NCLEX-style Questions
Question 1:
A patient with type 1 diabetes is admitted to the hospital with DKA. What is the nurse’s priority intervention?
A. Administering oral hypoglycemics
B. Initiating intravenous fluid replacement
C. Monitoring for signs of hyperglycemia
D. Educating the patient on diet modifications
Answer: B. Initiating intravenous fluid replacement is the priority intervention to correct dehydration and stabilize the patient in DKA.
Question 2:
A nurse is teaching a patient with type 2 diabetes about managing their condition. Which of the following lifestyle modifications is most important for maintaining stable blood glucose levels?
A. Regular physical activity
B. Avoiding all carbohydrates
C. Taking insulin only when blood sugar is high
D. Limiting fluid intake
Answer: A. Regular physical activity is important for maintaining stable blood glucose levels and overall health in patients with diabetes.
Question 3:
Which of the following findings would indicate that a patient is developing DKA?
A. Sudden weight gain and lethargy
B. Fruity breath and Kussmaul respirations
C. Pale skin and bradycardia
D. Low blood pressure and small pupils
Answer: B. Fruity breath and Kussmaul respirations (deep, labored breathing) are classic signs of DKA due to the accumulation of ketones and acidosis in the body.
CONCLUSION
Managing diabetes and preventing DKA requires vigilant monitoring, patient education, and timely interventions. Nurses play a critical role in ensuring that patients maintain optimal health and avoid complications through comprehensive care and support.