ASSESSING PEDIATRIC PAIN: TOOLS AND STRATEGIES FOR NURSES
Introduction
Pain is an inevitable part of life, but when it comes to children, evaluating and managing pain can be particularly challenging. Unlike adults, children may struggle to articulate their discomfort, making it essential for nurses to employ effective assessment tools and strategies. Accurate pain assessment not only alleviates suffering but also prevents potential long-term psychological effects. This blog delves into the various tools and strategies nurses can utilize to assess pediatric pain effectively.
Understanding the Challenges
Children’s developmental stages significantly influence their ability to express pain. Infants rely solely on behavioral cues, while toddlers might use basic language, and older children can provide more detailed descriptions. Additionally, cultural factors, previous medical experiences, and individual pain thresholds add layers of complexity to pain assessment in pediatric patients.
Pain Assessment Tools
1. Neonates and Infants (0-12 months):
• Neonatal Infant Pain Scale (NIPS): This tool evaluates facial expression, cry, breathing patterns, arm and leg movements, and arousal state to assess pain in neonates.
• FLACC Scale (Face, Legs, Activity, Cry, Consolability): Originally designed for infants, this scale observes five behavioral components to gauge pain levels.
2. Toddlers and Preschoolers (1-5 years):
• FLACC Scale: Continues to be effective in this age group, especially for those unable to verbalize their pain.
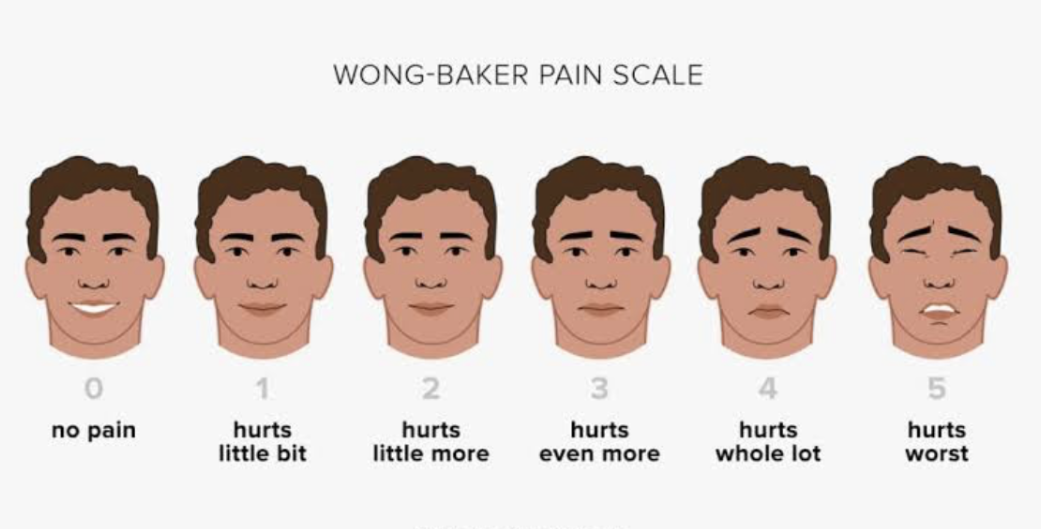
• Faces Pain Scale – Revised (FPS-R): Displays a series of faces ranging from a happy face (no pain) to a crying face (worst pain). Children point to the face that best represents their pain intensity.
3. School-Aged Children (6-12 years):
• Numeric Rating Scale (NRS): Children rate their pain on a scale from 0 (no pain) to 10 (worst possible pain). Suitable for children who can comprehend numerical concepts.
• Visual Analog Scale (VAS): A 10-centimeter line where one end signifies ‘no pain’ and the other ‘worst pain.’ The child marks a point on the line that corresponds to their pain level.
4. Adolescents (13-18 years):
• Numeric Rating Scale (NRS): Remains effective for this age group.
• Adolescent Pediatric Pain Tool (APPT): A multidimensional tool that assesses pain location, intensity, and quality, providing a comprehensive pain profile.
Strategies for Effective Pain Assessment
• Establish Rapport: Building trust with pediatric patients encourages them to express their pain more openly. A friendly demeanor and taking time to converse can make a significant difference.
• Involve Caregivers: Parents or guardians can offer valuable insights into their child’s pain behaviors and thresholds, aiding in a more accurate assessment.
• Use Age-Appropriate Language: Tailor your communication to the child’s developmental level. Avoid medical jargon and use simple, clear terms.
• Observe Non-Verbal Cues: Pay attention to facial expressions, body movements, and vocalizations, especially in non-verbal children.
• Regular Reassessment: Children’s pain levels can change rapidly. Frequent reassessment ensures timely interventions and adjustments to pain management plans.
Conclusion
Assessing pain in pediatric patients requires a blend of appropriate tools, keen observation, and effective communication. By understanding and implementing these strategies, nurses can ensure that children’s pain is accurately identified and managed, leading to better health outcomes and a more positive healthcare experience






