FLUID AND ELECTROLYTE IMBALANCES IN CHILDREN: NCLEX ESSENTIALS
Introduction:
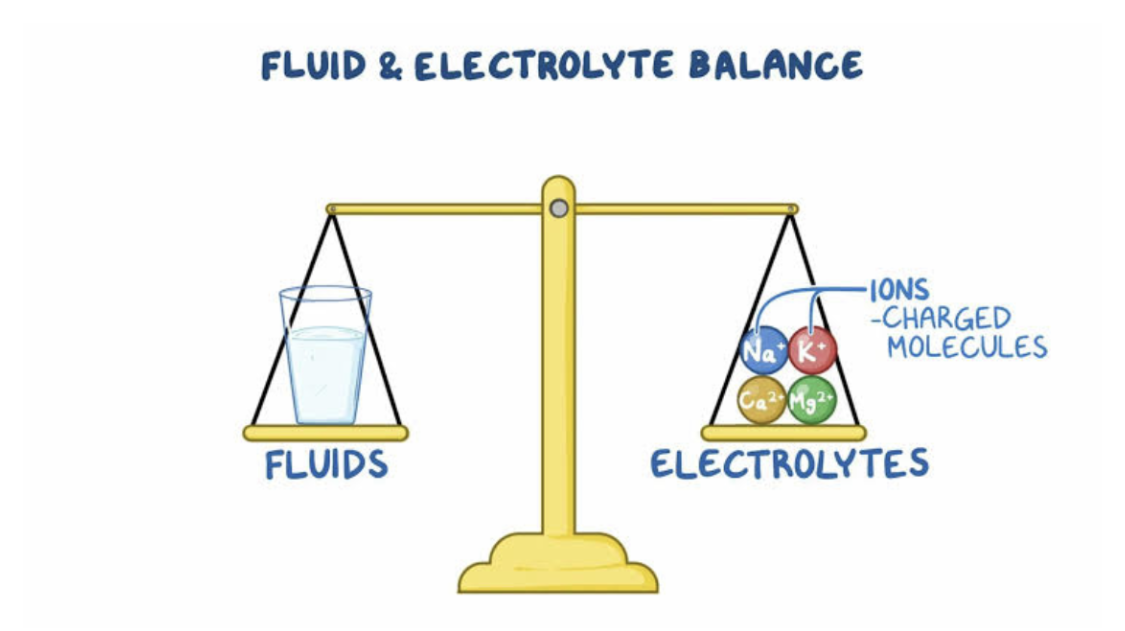
Children are not just small adults; their bodies have unique physiological differences that make them more susceptible to fluid and electrolyte imbalances. Rapid growth, higher metabolic rates, and a greater proportion of body water contribute to this vulnerability. For nursing professionals, especially those preparing for the NCLEX, understanding these nuances is crucial. This blog delves into the essentials of pediatric fluid and electrolyte imbalances, offering insights and practical knowledge to ensure optimal care for our youngest patients.
1. Why Are Children More Prone to Fluid and Electrolyte Imbalances?
Children’s bodies are like high-speed trains—everything moves faster. Their higher metabolic rates mean they produce more waste and lose fluids more quickly. Additionally, infants have a larger extracellular fluid volume, making them more susceptible to fluid shifts. Factors such as immature kidney function and a higher body surface area relative to weight also play significant roles. Recognizing these differences is the first step in preventing and managing imbalances.
2. Common Causes of Imbalances in Pediatrics:
Several factors can disrupt fluid and electrolyte balance in children:
• Gastrointestinal losses: Vomiting and diarrhea can rapidly deplete fluids and electrolytes.
• Fever: Increases insensible water loss through the skin and respiratory tract.
• Inadequate intake: Illness or difficulty feeding can lead to insufficient fluid consumption.
• Medical conditions: Diseases like diabetes or kidney disorders can affect fluid regulation.
Understanding these causes helps in early identification and intervention.
3. Recognizing Signs and Symptoms:
Timely detection of imbalances is vital. Symptoms can vary based on the specific electrolyte affected but may include:
• Dehydration: Dry mucous membranes, sunken fontanelles in infants, decreased urine output, and lethargy.
• Electrolyte disturbances: Muscle cramps, irregular heart rhythms, seizures, and altered mental status.
Regular monitoring and thorough assessments are key components of pediatric care.
4. Nursing Interventions:
Effective management involves a combination of monitoring, intervention, and education:
• Assessment: Regularly monitor vital signs, weight, and laboratory values.
• Fluid management: Administer oral rehydration solutions for mild dehydration; intravenous fluids may be necessary for severe cases.
• Electrolyte correction: Replace specific electrolytes as indicated, ensuring careful calculation to avoid rapid shifts.
• Parental education: Teach caregivers about signs of imbalances, the importance of hydration, and when to seek medical attention.
Collaboration with a multidisciplinary team ensures comprehensive care.
5. NCLEX Practice Questions:
To solidify your understanding, consider the following practice questions:
Question 1: An infant presents with severe diarrhea. Which assessment finding would indicate dehydration?
• A) Bulging fontanelle
• B) Moist mucous membranes
• C) Sunken eyes
• D) Increased urine output
Answer: C) Sunken eyes. This is a common sign of dehydration in infants.
Question 2: A child with vomiting and diarrhea is at risk for which electrolyte imbalance?
• A) Hyperkalemia
• B) Hypokalemia
• C) Hypernatremia
• D) Hypercalcemia
Answer: B) Hypokalemia. Gastrointestinal losses can lead to low potassium levels.
Question 3: Which intervention is appropriate for a child with mild dehydration?
• A) Administering intravenous fluids immediately
• B) Offering oral rehydration solutions
• C) Restricting fluids to prevent overhydration
• D) Providing caffeinated beverages
Answer: B) Offering oral rehydration solutions. This is the first-line treatment for mild dehydration.
Question 4: What is a key difference in fluid balance between children and adults?
• A) Children have a lower metabolic rate.
• B) Children have a higher proportion of body water.
• C) Adults have a higher body surface area relative to weight.
• D) Adults are more prone to fluid imbalances.
Answer: B) Children have a higher proportion of body water, making them more susceptible to fluid shifts.
Conclusion:
Understanding fluid and electrolyte imbalances in children is a cornerstone of pediatric nursing. By recognizing the unique aspects of pediatric physiology and implementing targeted interventions, nurses can effectively manage these conditions. Continuous learning and practice, including NCLEX-style questions, will prepare nursing professionals to provide the highest standard of care to their young patients.






