CONGENITAL HEART DEFECTS IN CHILDREN: NCLEX-STYLE QUESTIONS AND KEY NURSING INTERVENTIONS
Congenital heart defects (CHDs) are structural anomalies of the heart present at birth, affecting normal blood flow and posing significant challenges in pediatric care. For nursing professionals, understanding these defects and their management is crucial, especially when preparing for licensure exams like the NCLEX. This article delves into common CHDs, essential nursing interventions, and includes NCLEX-style questions to enhance comprehension.
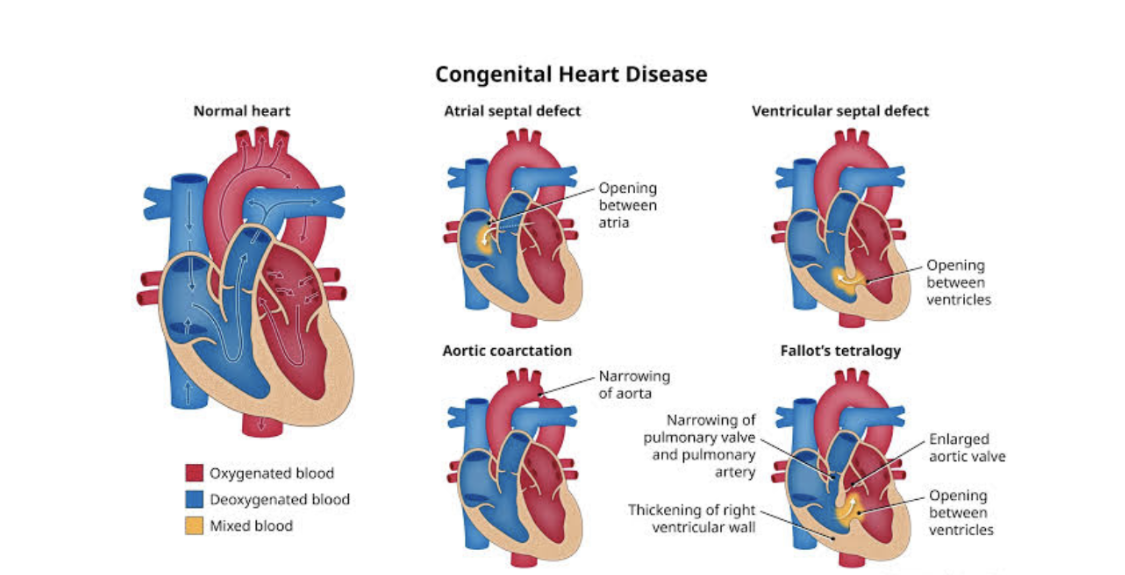
Understanding Congenital Heart Defects
CHDs encompass a variety of structural heart problems that arise during fetal development. They can be broadly categorized based on their impact on pulmonary blood flow:
1. Increased Pulmonary Blood Flow Defects: Conditions where blood is shunted from the left side of the heart to the right, leading to excessive blood flow to the lungs. Examples include:
• Atrial Septal Defect (ASD): An opening in the atrial septum allowing blood to flow between the left and right atria.
• Ventricular Septal Defect (VSD): A hole in the ventricular septum permitting blood flow between the left and right ventricles.
2. Decreased Pulmonary Blood Flow Defects: Conditions causing reduced blood flow to the lungs, often leading to cyanosis. An example is:
• Tetralogy of Fallot: A combination of four defects: VSD, pulmonary stenosis, right ventricular hypertrophy, and an overriding aorta.
Key Nursing Interventions
Effective nursing care for children with CHDs involves comprehensive assessment, vigilant monitoring, and family education. Essential interventions include:
• Monitoring Vital Signs: Regularly assess heart rate, respiratory rate, blood pressure, and oxygen saturation to detect changes indicative of hemodynamic instability.
• Auscultation: Listen for heart murmurs or abnormal lung sounds, which may signal complications like heart failure or pulmonary congestion.
• Assessing for Cyanosis: Observe skin, lips, and nail beds for bluish discoloration, indicating hypoxemia.
• Promoting Optimal Nutrition: Provide small, frequent feedings to reduce the metabolic demand on the heart and ensure adequate caloric intake.
• Educating Families: Offer clear information about the child’s condition, treatment plan, and signs of potential complications to empower caregivers in managing the child’s health.
NCLEX-Style Practice Questions
1. Question: A 3-month-old infant with a known ventricular septal defect presents with poor feeding, tachypnea, and diaphoresis during feeds. Which nursing intervention is most appropriate?
Answer: Offer small, frequent feedings with increased caloric density to meet nutritional needs without overexerting the infant.
2. Question: During a routine assessment, a nurse notes a machinery-like murmur in a 2-week-old neonate. This finding is most indicative of which congenital heart defect?
Answer: Patent Ductus Arteriosus (PDA).
3. Question: A child with Tetralogy of Fallot experiences a hypercyanotic spell. Which immediate action should the nurse take?
Answer: Place the child in a knee-chest position to increase systemic vascular resistance and improve oxygenation.
4. Question: Parents of an infant diagnosed with an atrial septal defect ask about the necessity of surgical intervention. The nurse’s best response is:
Answer: “Many small ASDs close spontaneously; however, larger defects may require surgical repair to prevent complications.”
5. Question: Which of the following is a priority nursing diagnosis for a child with a congenital heart defect experiencing decreased cardiac output?
Answer: Activity intolerance related to imbalance between oxygen supply and demand.
Understanding congenital heart defects and their management is vital for nursing professionals. Through diligent assessment, targeted interventions, and continuous education, nurses play a pivotal role in optimizing outcomes for pediatric patients with CHDs.






