Acute Respiratory Distress Syndrome (ARDS): A Guide for NCLEX Exam Preparation
Acute Respiratory Distress Syndrome (ARDS) is a critical condition that nursing students must thoroughly understand for the NCLEX exam. ARDS is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Understanding the causes, pathophysiology, clinical manifestations, management, and nursing interventions for ARDS is essential for providing appropriate care and achieving success on the NCLEX.
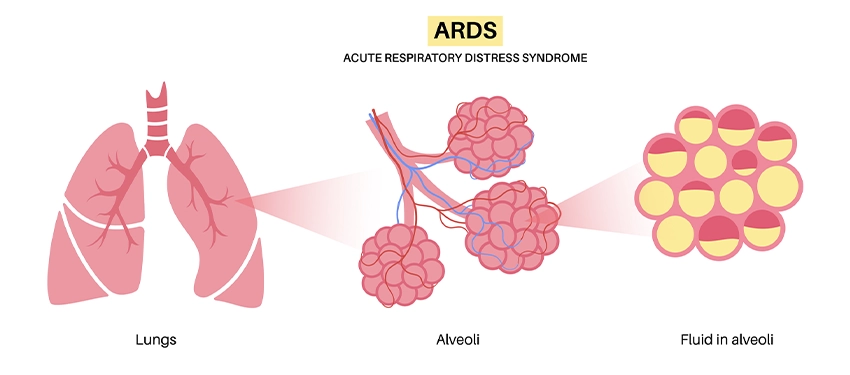
What is ARDS?
ARDS is a severe lung condition that occurs when fluid builds up in the alveoli (air sacs) of the lungs. This fluid prevents the lungs from filling with enough air, leading to reduced oxygen levels in the bloodstream. ARDS can result from various direct or indirect injuries to the lungs, including pneumonia, sepsis, trauma, or inhalation of harmful substances.
Causes of ARDS
- Sepsis: The most common cause of ARDS, particularly when the infection spreads to the lungs.
- Pneumonia: Severe lung infections can trigger an inflammatory response, leading to ARDS.
- Aspiration: Inhalation of stomach contents, food, or water can cause direct lung injury.
- Trauma: Major injuries, especially to the chest or head, can lead to ARDS.
- Pancreatitis: Severe inflammation of the pancreas can release enzymes and inflammatory mediators that damage the lungs.
- Inhalation Injury: Breathing in harmful substances like smoke, chemicals, or saltwater can directly injure the lungs.
- Blood Transfusions: Multiple or massive blood transfusions can sometimes lead to ARDS.
Pathophysiology of ARDS
ARDS is characterized by three phases:
- Exudative Phase:
- Occurs within the first 1-7 days after the initial injury.
- Inflammation causes damage to the alveolar-capillary membrane, leading to increased permeability.
- Fluid, proteins, and inflammatory cells leak into the alveoli, causing pulmonary edema.
- Surfactant production decreases, leading to alveolar collapse (atelectasis).
- Proliferative Phase:
- Occurs 1-2 weeks after the injury.
- Lung tissue starts to repair itself, with fibroblast proliferation and formation of scar tissue.
- The lung becomes less compliant, and gas exchange continues to be impaired.
- Fibrotic Phase:
- Occurs 2-3 weeks after the injury.
- Extensive fibrosis and scarring occur, leading to further stiffening of the lungs and chronic respiratory insufficiency.
Clinical Manifestations
- Severe Dyspnea: Rapid onset of breathing difficulty, often requiring supplemental oxygen or mechanical ventilation.
- Hypoxemia: Low levels of oxygen in the blood, unresponsive to increased oxygen delivery (refractory hypoxemia).
- Tachypnea: Rapid breathing as the body attempts to compensate for low oxygen levels.
- Cyanosis: Bluish discoloration of the skin and mucous membranes due to low oxygen saturation.
- Crackles: Abnormal lung sounds heard on auscultation, indicating fluid in the alveoli.
- Respiratory Distress: Use of accessory muscles, nasal flaring, and intercostal retractions as the patient struggles to breathe.
- Decreased Lung Compliance: The lungs become stiff, making it difficult to ventilate.
Diagnostic Criteria
The Berlin criteria are used to diagnose ARDS:
- Timing: Acute onset within 1 week of a known clinical insult or new/worsening respiratory symptoms.
- Chest Imaging: Bilateral opacities on chest X-ray or CT scan not fully explained by effusions, lobar/lung collapse, or nodules.
- Origin of Edema: Respiratory failure not fully explained by cardiac failure or fluid overload; objective assessment (e.g., echocardiography) is needed to rule out hydrostatic edema if no risk factors are present.
- Oxygenation: Hypoxemia is assessed by the PaO2/FiO2 ratio, with the following classifications:
- Mild: 200 < PaO2/FiO2 ≤ 300 mmHg with PEEP or CPAP ≥ 5 cm H2O
- Moderate: 100 < PaO2/FiO2 ≤ 200 mmHg with PEEP ≥ 5 cm H2O
- Severe: PaO2/FiO2 ≤ 100 mmHg with PEEP ≥ 5 cm H2O
Management of ARDS
- Mechanical Ventilation:
- Low Tidal Volume Ventilation: To reduce the risk of barotrauma and volutrauma, low tidal volumes (4-6 mL/kg of ideal body weight) are used.
- Positive End-Expiratory Pressure (PEEP): Helps keep the alveoli open, improving oxygenation.
- Prone Positioning: Repositioning the patient from their back to their stomach can improve oxygenation and reduce ventilator-associated lung injury.
- High-Frequency Oscillatory Ventilation (HFOV): May be used in severe cases when conventional ventilation fails.
- Fluid Management:
- Conservative fluid management strategies are preferred to prevent worsening pulmonary edema.
- Diuretics may be used to manage fluid balance.
- Pharmacologic Therapy:
- Corticosteroids: May be used to reduce inflammation, especially in the proliferative and fibrotic phases.
- Antibiotics: Administered if the underlying cause is infection (e.g., sepsis or pneumonia).
- Neuromuscular Blockade: Used in the early phase of severe ARDS to improve oxygenation and ventilation synchrony.
- Supportive Care:
- Ensure adequate nutrition, often via enteral feeding, to support healing and prevent muscle wasting.
- Prevent complications such as ventilator-associated pneumonia (VAP) through proper infection control measures.
Nursing Interventions for ARDS
- Monitor Respiratory Status:
- Frequently assess lung sounds, respiratory rate, and oxygen saturation.
- Monitor ABGs (arterial blood gases) to assess the effectiveness of ventilation and oxygenation.
- Optimize Oxygenation and Ventilation:
- Maintain the patient in a semi-Fowler’s position to facilitate breathing.
- Implement prone positioning as prescribed.
- Ensure the mechanical ventilator settings are appropriate for the patient’s condition.
- Fluid and Electrolyte Management:
- Monitor fluid intake and output, and adjust fluid administration as needed.
- Monitor electrolyte levels, especially potassium and sodium, to prevent imbalances.
- Prevent Complications:
- Implement strategies to prevent VAP, including oral care and elevating the head of the bed.
- Use stress ulcer prophylaxis and deep vein thrombosis (DVT) prophylaxis as ordered.
- Provide Emotional Support:
- Offer reassurance and explanations to the patient and their family.
- Address anxiety and fear related to the severity of the condition.
Sample NCLEX Questions
Question 1
A patient with ARDS is being treated with mechanical ventilation. The nurse notes that the patient is receiving low tidal volume ventilation. What is the primary rationale for this intervention?
A. To reduce the risk of oxygen toxicity
B. To prevent the development of pulmonary emboli
C. To minimize the risk of barotrauma and volutrauma
D. To improve carbon dioxide elimination
Answer: C. To minimize the risk of barotrauma and volutrauma
Question 2
The nurse is caring for a patient with ARDS who is on a ventilator. Which of the following interventions would be appropriate to improve oxygenation?
A. Position the patient in high Fowler’s position.
B. Increase the patient’s tidal volume to 10 mL/kg.
C. Administer a diuretic to reduce fluid overload.
D. Place the patient in a prone position.
Answer: D. Place the patient in a prone position.
Question 3
A patient with ARDS is receiving PEEP on a mechanical ventilator. What is the primary purpose of this therapy?
A. To increase tidal volume
B. To improve alveolar recruitment
C. To reduce respiratory rate
D. To lower oxygen requirements
Answer: B. To improve alveolar recruitment
NCLEX Preparation Tips for ARDS
- Understand the Pathophysiology: Focus on the mechanisms of lung injury in ARDS and how they lead to respiratory failure.
- Know the Diagnostic Criteria: Be familiar with the Berlin criteria for diagnosing ARDS, as this is often tested on the NCLEX.
- Learn the Interventions: Understand the rationale behind each intervention, especially mechanical ventilation strategies like low tidal volume ventilation and PEEP.
- Practice NCLEX Questions: Regularly practice questions related to ARDS to reinforce your understanding of the condition and its management.






