Comprehensive Care for a Client with Upper Gastrointestinal Tract Health Problems: An NCLEX-Standard Guide
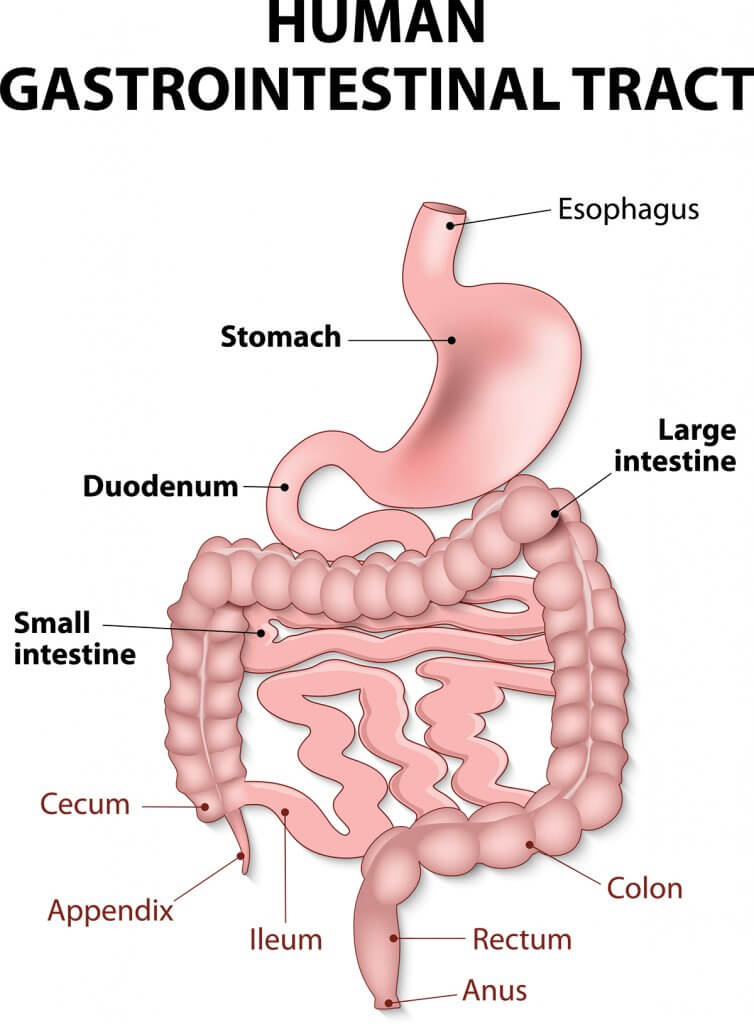
Upper gastrointestinal (GI) tract health problems encompass a range of conditions affecting the esophagus, stomach, and duodenum. These issues can significantly impact a patient’s quality of life and overall health. This guide, aligned with NCLEX standards, covers the essential aspects of managing a client with upper GI tract problems, including assessment, common conditions, treatment options, nursing interventions, and patient education.
Understanding Upper Gastrointestinal Tract Problems
The upper GI tract includes the esophagus, stomach, and duodenum. Common health problems in this area include gastroesophageal reflux disease (GERD), peptic ulcer disease (PUD), gastritis, and esophageal varices.
Common Symptoms
Symptoms of upper GI tract problems can vary but often include:
- Heartburn or acid reflux
- Epigastric pain or discomfort
- Nausea and vomiting
- Bloating
- Dysphagia (difficulty swallowing)
- Hematemesis (vomiting blood)
- Melena (black, tarry stools)
Common Conditions
1. Gastroesophageal Reflux Disease (GERD)
Symptoms:
- Persistent heartburn
- Acid regurgitation
- Chest pain
- Difficulty swallowing
- Chronic cough
Treatment:
- Lifestyle modifications (diet changes, weight loss, elevating the head of the bed)
- Medications (antacids, H2 receptor blockers, proton pump inhibitors)
- Surgical intervention (Nissen fundoplication) in severe cases
2. Peptic Ulcer Disease (PUD)
Symptoms:
- Epigastric pain (often relieved by eating)
- Nausea and vomiting
- Bloating
- Hematemesis or melena
Treatment:
- Medications (proton pump inhibitors, H2 receptor blockers, antibiotics for H. pylori infection)
- Lifestyle changes (avoiding NSAIDs, alcohol, smoking)
- Surgical intervention in severe or complicated cases
3. Gastritis
Symptoms:
- Epigastric pain or discomfort
- Nausea and vomiting
- Bloating
- Loss of appetite
Treatment:
- Medications (antacids, H2 receptor blockers, proton pump inhibitors, antibiotics for H. pylori infection)
- Dietary changes (avoiding irritants like spicy foods, alcohol, caffeine)
- Stress management
4. Esophageal Varices
Symptoms:
- Hematemesis
- Melena
- Signs of liver disease (jaundice, ascites, spider angiomas)
Treatment:
- Medications (beta-blockers to reduce portal hypertension)
- Endoscopic procedures (banding or sclerotherapy)
- Management of underlying liver disease
- Emergency care for variceal bleeding (IV fluids, blood transfusions)
Nursing Care and Considerations
1. Comprehensive Assessment
- History Taking: Obtain a detailed medical history, including previous GI issues, medication use, lifestyle factors, and family history.
- Physical Examination: Perform a thorough physical exam, focusing on the abdomen and any signs of GI distress.
- Diagnostic Tests: Ensure completion of necessary tests such as endoscopy, barium swallow, H. pylori testing, and liver function tests.
2. Symptom Management
- Pain Control: Regularly assess pain levels and administer prescribed pain relief medications.
- Nausea and Vomiting: Administer antiemetics and provide dietary recommendations to manage symptoms.
- Bleeding: Monitor for signs of GI bleeding and intervene promptly if detected.
3. Patient Education
- Dietary Changes: Educate on the importance of a diet that avoids irritants and supports healing (e.g., small, frequent meals, avoiding spicy and acidic foods).
- Medication Adherence: Emphasize the importance of taking prescribed medications as directed and understanding potential side effects.
- Lifestyle Modifications: Encourage weight management, smoking cessation, and reducing alcohol intake.
4. Psychological Support
- Emotional Support: Provide a supportive environment and address any anxieties or fears the client may have.
- Counseling: Refer to counseling services if needed to help cope with chronic illness.
5. Monitoring and Follow-Up
- Regular Monitoring: Monitor vital signs, lab results, and symptoms regularly to detect any changes in condition.
- Follow-Up Appointments: Ensure the client attends follow-up appointments for ongoing assessment and treatment adjustments.
Case Study: Managing a Client with Peptic Ulcer Disease
Background
Mr. Smith, a 55-year-old male, presents with epigastric pain that is relieved by eating and a history of NSAID use for chronic back pain. He has been experiencing nausea and occasional vomiting.
Assessment
- History: Detailed history of symptoms, NSAID use, lifestyle factors, and family history of GI conditions.
- Physical Exam: Epigastric tenderness noted on palpation.
- Diagnostic Tests: Endoscopy reveals a duodenal ulcer; H. pylori test is positive.
Treatment Plan
- Medications:
- Proton pump inhibitor (PPI) to reduce stomach acid
- Antibiotics to eradicate H. pylori infection
- Discontinuation of NSAIDs
- Lifestyle Modifications:
- Dietary changes to avoid irritants
- Smoking cessation
- Stress management techniques
Nursing Interventions
- Education: Provided detailed instructions on medication regimen, dietary changes, and lifestyle modifications.
- Symptom Management: Administered prescribed medications and monitored for side effects.
- Follow-Up: Scheduled follow-up appointment to reassess symptoms and effectiveness of treatment.
Nursing Considerations
1. Pain Management
- Assessment: Regularly assess pain using standardized pain scales and adjust pain management strategies as needed.
- Interventions: Administer prescribed pain medications and provide non-pharmacological pain relief methods.
2. Infection Prevention
- Medication Adherence: Ensure the client completes the full course of antibiotics for H. pylori infection.
- Hygiene Practices: Educate on proper hygiene to prevent reinfection.
3. Nutrition and Hydration
- Dietary Support: Provide dietary recommendations to support healing and manage symptoms.
- Hydration: Encourage adequate fluid intake to prevent dehydration.
Conclusion
Managing upper gastrointestinal tract health problems requires a comprehensive approach that includes thorough assessment, effective symptom management, patient education, and psychological support. Nurses play a crucial role in providing holistic care that promotes healing and improves quality of life for clients with upper GI conditions. By adhering to NCLEX standards, nurses can ensure they are delivering high-quality, evidence-based care to their clients.






