IMMUNE AND INFEXTIOUS DISEASES: HIV/AIDS, SEPSIS, AND ISOLATION PROTOCOLS
Introduction:
Immune and infectious diseases represent a significant challenge in healthcare, requiring a nuanced understanding of pathophysiology, prevention, and management. HIV/AIDS and sepsis, in particular, are critical areas of focus due to their life-altering implications and high mortality rates. Additionally, adherence to isolation protocols is essential to controlling the spread of infectious agents in healthcare and community settings. This blog will explore these topics, providing accurate, research-backed insights to enhance understanding and improve care delivery.
Understanding HIV/AIDS
Human Immunodeficiency Virus (HIV) is a retrovirus that attacks the immune system, specifically targeting CD4 cells, weakening the body’s ability to fight infections and diseases. Acquired Immunodeficiency Syndrome (AIDS) is the most advanced stage of HIV, marked by a severely compromised immune system and the emergence of opportunistic infections.
Transmission and Prevention:
HIV spreads through specific bodily fluids such as blood, semen, vaginal secretions, and breast milk. Common modes of transmission include unprotected sexual contact, sharing needles, and from mother to child during childbirth or breastfeeding. Prevention strategies include:
• Consistent use of condoms and practicing safe sex.
• Regular HIV testing and knowing one’s status.
• Use of Pre-Exposure Prophylaxis (PrEP) for high-risk individuals.
• Avoiding needle sharing and adhering to universal precautions.
Management and Treatment:
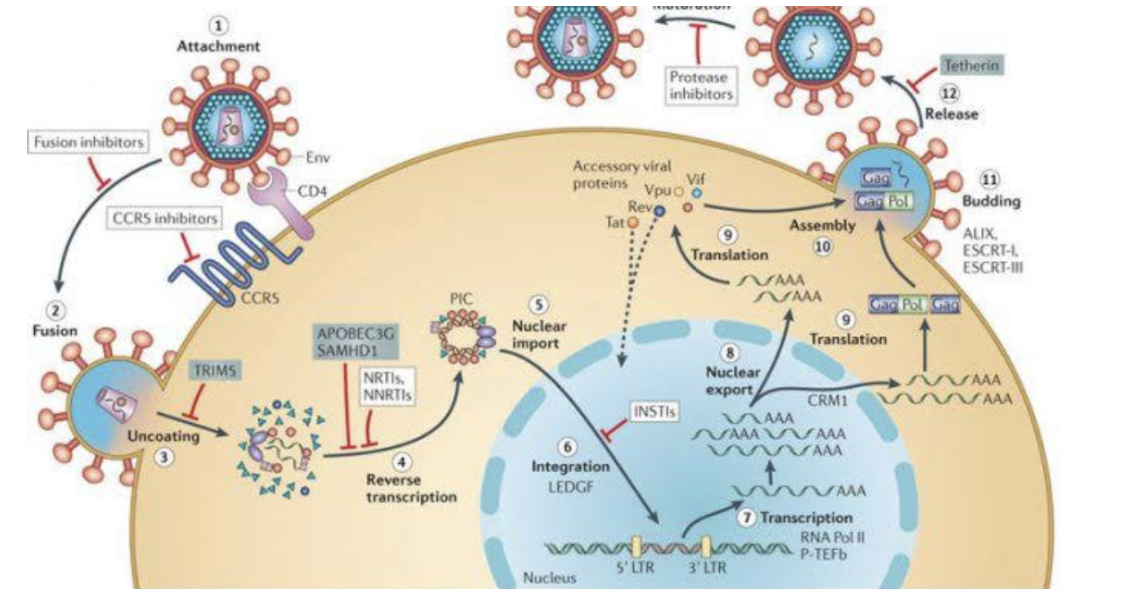
While there is no cure for HIV, antiretroviral therapy (ART) is highly effective in managing the virus and preventing progression to AIDS. ART works by suppressing viral replication, maintaining a healthy immune system, and reducing the risk of transmission. Early diagnosis and consistent treatment adherence are critical for successful management.
Understanding Sepsis
Sepsis is a life-threatening condition that arises when the body’s response to infection triggers widespread inflammation, leading to tissue damage, organ failure, or death. It is a medical emergency requiring immediate recognition and intervention.
Symptoms and Early Recognition:
Sepsis can develop rapidly, and early recognition is essential. Symptoms include:
• Fever or hypothermia.
• Rapid heart rate and breathing.
• Altered mental state or confusion.
• Low blood pressure and reduced urine output.
Prompt identification using tools such as the Sepsis-3 criteria or the quick SOFA (qSOFA) score can improve outcomes.
Treatment Strategies:
The cornerstone of sepsis management is the “Sepsis Six” bundle, which includes:
1. Administering high-flow oxygen.
2. Taking blood cultures.
3. Administering broad-spectrum antibiotics.
4. Starting IV fluid resuscitation.
5. Measuring lactate levels.
6. Monitoring urine output.
Timely administration of antibiotics and hemodynamic support are critical to improving survival rates.
Isolation Protocols in Healthcare
Isolation protocols are implemented to control the spread of infectious diseases. They vary depending on the mode of transmission—contact, droplet, or airborne—and are essential for protecting both patients and healthcare workers.
Types of Isolation Precautions:
• Standard Precautions: Applied to all patients to prevent transmission of pathogens through blood, body fluids, and mucous membranes.
• Contact Precautions: Used for infections spread by direct or indirect contact, such as MRSA or Clostridioides difficile.
• Droplet Precautions: For diseases spread by respiratory droplets, including influenza and pertussis.
• Airborne Precautions: Required for diseases like tuberculosis and measles, involving pathogens that remain infectious over long distances.
Key Practices:
• Hand hygiene is the most effective way to prevent infection.
• Use of personal protective equipment (PPE) such as gloves, gowns, masks, or respirators depending on the level of isolation required.
• Proper patient placement, such as negative pressure rooms for airborne diseases.
• Adherence to strict environmental cleaning protocols.
Questions and Answers:
Question 1: What are the primary modes of HIV transmission, and how can they be prevented?
Answer: HIV is primarily transmitted through unprotected sexual contact, sharing needles, blood transfusions, and from mother to child during childbirth or breastfeeding. Prevention strategies include using condoms, regular testing, taking PrEP if at high risk, and adhering to universal precautions in healthcare settings.
Question 2: What are some early signs of sepsis, and why is early intervention critical?
Answer: Early signs of sepsis include fever, rapid heart rate, confusion, and low blood pressure. Early intervention with antibiotics and fluids is crucial to prevent organ failure and reduce mortality.
Question 3: What is the difference between contact, droplet, and airborne precautions?
Answer: Contact precautions prevent diseases spread through direct or indirect contact, droplet precautions target infections transmitted by respiratory droplets, and airborne precautions address pathogens that remain infectious over long distances, such as tuberculosis.
Conclusion:
HIV/AIDS, sepsis, and isolation protocols are critical areas of focus in infectious disease management. Understanding transmission, prevention, and treatment options for HIV/AIDS, recognizing early signs of sepsis, and implementing effective isolation protocols can significantly improve patient outcomes. Through education and adherence to best practices, healthcare professionals can play a pivotal role in managing these complex conditions and preventing the spread of infectious diseases






