Pancreatitis: A Comprehensive Guide for NCLEX Exam Preparation
Pancreatitis, an inflammation of the pancreas, is a critical condition that nursing students need to understand thoroughly for the NCLEX exam. This guide will cover the causes, symptoms, diagnosis, management, and nursing care of pancreatitis, with a focus on both acute and chronic forms of the disease. We will also include sample NCLEX questions to help reinforce key concepts.
What is Pancreatitis?
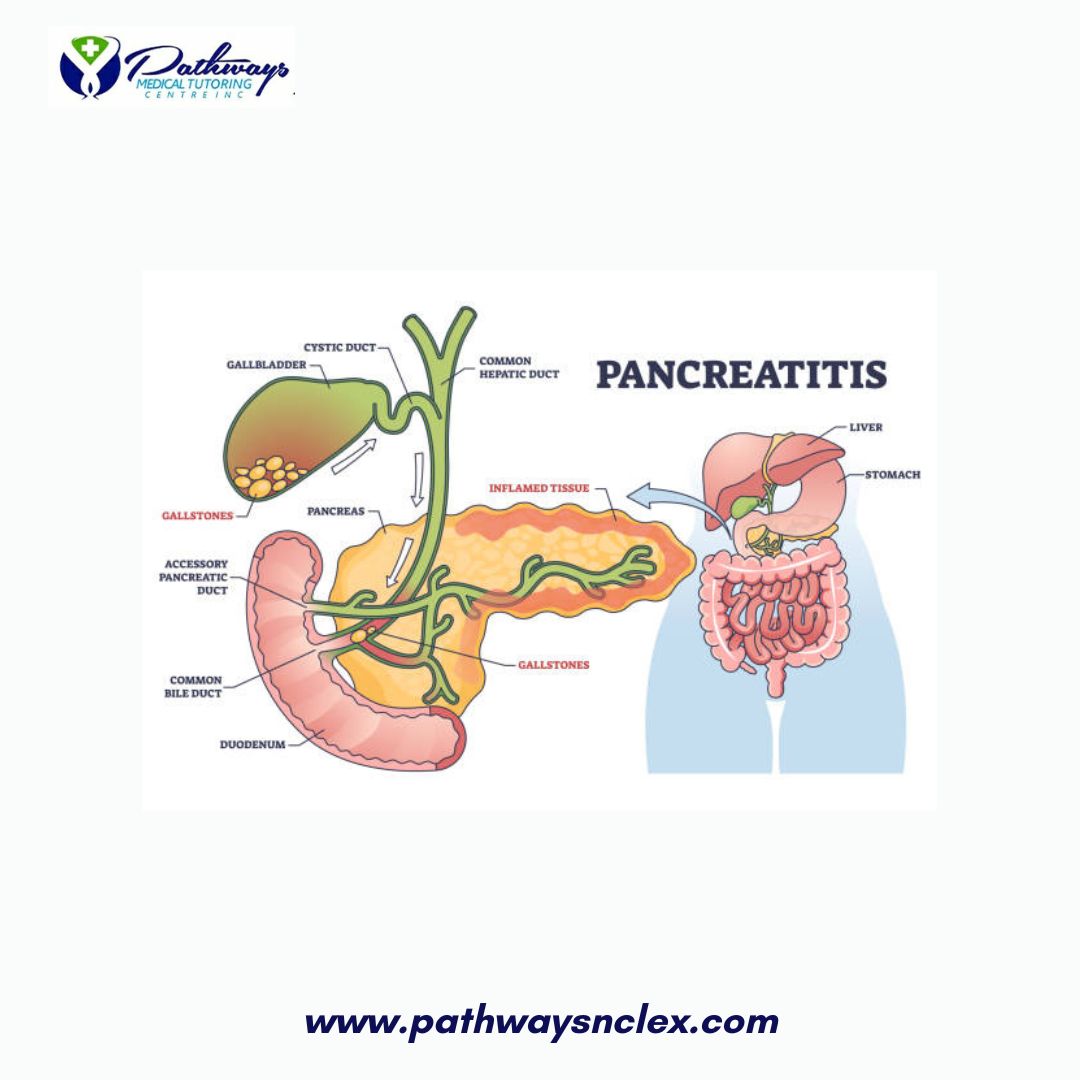
Pancreatitis occurs when digestive enzymes activate within the pancreas, causing inflammation and damage to the pancreatic tissue. It can be acute, with a sudden onset and severe symptoms, or chronic, with long-term damage leading to loss of pancreatic function.
Causes of Pancreatitis
The causes of pancreatitis can vary, but the most common include:
- Gallstones: The most frequent cause of acute pancreatitis, where stones block the bile duct, leading to enzyme backup.
- Alcohol Abuse: A leading cause of chronic pancreatitis and a common cause of acute pancreatitis in adults.
- Medications: Certain drugs, such as corticosteroids, thiazide diuretics, and azathioprine, can trigger pancreatitis.
- Hypertriglyceridemia: Extremely high levels of triglycerides in the blood can cause acute pancreatitis.
- Trauma: Injury to the abdomen or procedures like endoscopic retrograde cholangiopancreatography (ERCP) can lead to pancreatitis.
- Infections: Viral infections such as mumps or hepatitis can sometimes cause pancreatitis.
- Genetic Factors: Mutations in genes like PRSS1 or CFTR can increase the risk of developing pancreatitis.
- Autoimmune Conditions: Autoimmune pancreatitis occurs when the body’s immune system attacks the pancreas.
Symptoms of Pancreatitis
The symptoms of pancreatitis can differ depending on whether the condition is acute or chronic.
Acute Pancreatitis
- Severe Abdominal Pain: Often the first and most prominent symptom, typically in the upper abdomen and radiating to the back.
- Nausea and Vomiting: Common, especially after eating.
- Fever: Indicating inflammation and possible infection.
- Tachycardia: Increased heart rate due to pain and systemic inflammation.
- Jaundice: Yellowing of the skin and eyes if the bile duct is blocked by gallstones.
- Abdominal Tenderness: The abdomen may be swollen and tender to touch.
Chronic Pancreatitis
- Chronic Abdominal Pain: Persistent or recurrent pain in the upper abdomen.
- Malabsorption: Due to the pancreas’ inability to produce digestive enzymes, leading to weight loss and fatty stools (steatorrhea).
- Diabetes Mellitus: Over time, damage to insulin-producing cells can lead to diabetes.
- Jaundice: Less common but can occur if there is bile duct obstruction.
- Calcification: Visible on imaging studies, indicating chronic damage.
Diagnosis of Pancreatitis
Diagnosing pancreatitis involves a combination of clinical evaluation, laboratory tests, and imaging studies.
- Serum Amylase and Lipase: Elevated levels of these pancreatic enzymes are key indicators of pancreatitis, with lipase being more specific.
- Liver Function Tests: May show elevated bilirubin and alkaline phosphatase if the bile duct is blocked.
- Complete Blood Count (CBC): Leukocytosis (elevated white blood cell count) is common in acute pancreatitis.
- C-reactive Protein (CRP): Elevated CRP levels indicate inflammation.
- Imaging Studies:
- Ultrasound: Often used first to check for gallstones.
- CT Scan: Provides detailed images of the pancreas and can show inflammation, necrosis, or abscesses.
- MRI: May be used to assess complications and chronic changes.
- ERCP: Used to diagnose and sometimes treat causes of pancreatitis, such as bile duct obstructions.
Management of Pancreatitis
The management of pancreatitis focuses on relieving symptoms, preventing complications, and addressing the underlying cause.
Acute Pancreatitis
- NPO (Nothing by Mouth): To rest the pancreas, patients are kept NPO, and fluids are given intravenously.
- IV Fluids: Aggressive fluid resuscitation is essential to prevent dehydration and support circulation.
- Pain Management: Analgesics, such as morphine or hydromorphone, are used to control severe pain.
- Nutritional Support: Once symptoms improve, a gradual reintroduction of oral intake is started, often with a low-fat diet.
- Antibiotics: Used if there is evidence of infection, such as infected pancreatic necrosis.
- ERCP: May be necessary to remove gallstones or relieve bile duct obstructions.
Chronic Pancreatitis
- Pain Management: Long-term pain control is crucial, often requiring opioid analgesics and sometimes nerve blocks.
- Pancreatic Enzyme Supplements: Given to aid digestion and reduce steatorrhea.
- Insulin Therapy: May be needed if diabetes develops due to pancreatic damage.
- Dietary Modifications: A low-fat diet, avoiding alcohol, and small, frequent meals are recommended.
- Surgical Options: In some cases, surgery may be needed to remove part of the pancreas, drain cysts, or relieve bile duct obstructions.
Nursing Care for Pancreatitis
Nursing care for pancreatitis focuses on managing symptoms, preventing complications, and providing patient education.
Acute Pancreatitis
- Monitor Vital Signs: Regularly assess for signs of shock, such as hypotension and tachycardia.
- Pain Assessment: Continuously evaluate pain levels and administer analgesics as prescribed.
- Maintain NPO Status: Ensure the patient is kept NPO as ordered and administer IV fluids.
- Monitor for Complications: Be alert for signs of pancreatic necrosis, infection, or respiratory distress (ARDS).
- Patient Education: Teach patients about the importance of follow-up care and avoiding alcohol and high-fat foods.
Chronic Pancreatitis
- Nutritional Support: Work with a dietitian to provide appropriate dietary advice, emphasizing small, frequent, low-fat meals.
- Pain Management: Help patients manage chronic pain through medications, lifestyle changes, and alternative therapies.
- Monitor for Diabetes: Regularly check blood glucose levels and educate patients on managing diabetes if it develops.
- Psychosocial Support: Chronic pancreatitis can be debilitating; provide emotional support and resources for coping with long-term illness.
Sample NCLEX Questions
Question 1
A patient with acute pancreatitis is complaining of severe abdominal pain radiating to the back. Which of the following interventions should the nurse implement first?
A. Administer morphine as prescribed.
B. Encourage the patient to walk around.
C. Start an IV infusion of normal saline.
D. Insert a nasogastric tube for decompression.
Answer: A. Administer morphine as prescribed.
Question 2
Which of the following laboratory results is most indicative of acute pancreatitis?
A. Elevated serum creatinine
B. Elevated serum lipase
C. Elevated serum potassium
D. Elevated serum bilirubin
Answer: B. Elevated serum lipase
Question 3
A patient with chronic pancreatitis is experiencing steatorrhea and weight loss. Which intervention should the nurse include in the plan of care?
A. Encourage a high-fat diet to compensate for weight loss.
B. Administer pancreatic enzyme supplements with meals.
C. Restrict fluids to reduce gastrointestinal symptoms.
D. Administer antibiotics to prevent infection.
Answer: B. Administer pancreatic enzyme supplements with meals.
NCLEX Preparation Tips for Pancreatitis
- Understand the Pathophysiology: Focus on how the activation of pancreatic enzymes leads to inflammation and damage.
- Know the Differences: Be able to differentiate between acute and chronic pancreatitis, particularly in terms of symptoms, management, and complications.
- Practice Nursing Interventions: Review nursing care plans and interventions for managing pain, monitoring for complications, and providing nutritional support.
Conclusion
Pancreatitis is a complex condition that requires comprehensive nursing care to manage symptoms and prevent complications. By understanding the causes, symptoms, and treatments of both acute and chronic pancreatitis, nursing students can be better prepared for the NCLEX exam and their future roles in patient care.






