Parkinson’s Disease: Causes, Symptoms, and Care – NCLEX Guide
Parkinson’s disease (PD) is a chronic and progressive neurodegenerative disorder that primarily affects movement control. As a nursing student preparing for the NCLEX exam, it is crucial to understand the causes, symptoms, and nursing care associated with Parkinson’s disease to provide comprehensive care and improve patient outcomes.
What is Parkinson’s Disease?
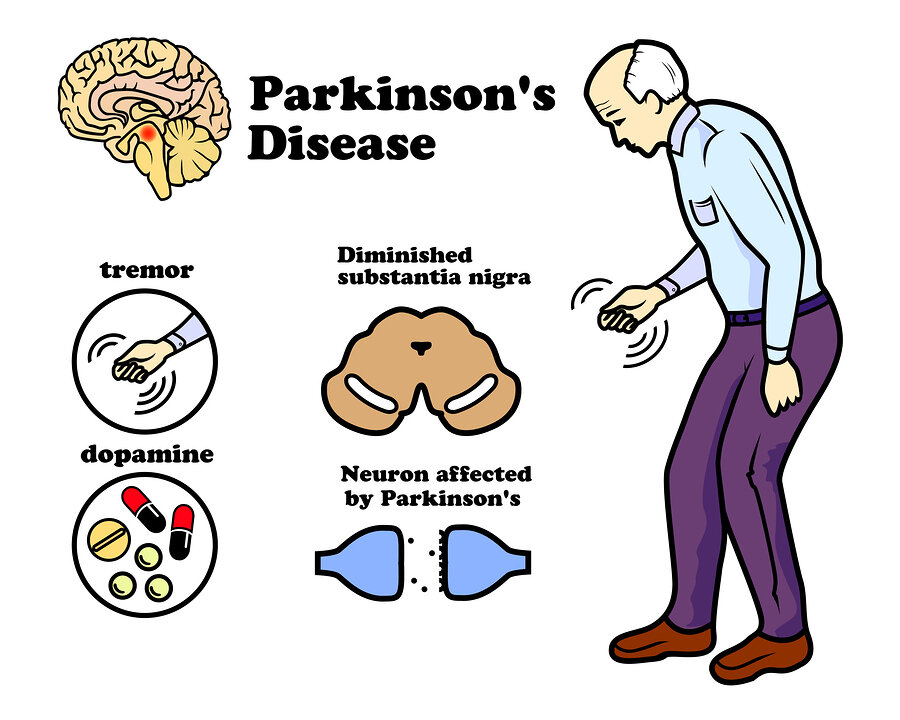
Parkinson’s disease is a neurodegenerative disorder that affects the motor system, leading to symptoms like tremors, bradykinesia (slowness of movement), and rigidity. It is caused by the progressive loss of dopamine-producing neurons in the substantia nigra, a part of the brain that controls movement.
Causes of Parkinson’s Disease
The exact cause of Parkinson’s disease is unknown, but several factors are believed to contribute to its development:
- Genetics: Mutations in certain genes (e.g., LRRK2, PARK7, PINK1, SNCA) are associated with familial Parkinson’s disease. However, these cases are rare.
- Environmental Factors: Exposure to toxins such as pesticides, herbicides, and heavy metals has been linked to an increased risk of developing Parkinson’s disease.
- Age: Parkinson’s disease is more common in older adults, typically developing after the age of 60.
- Gender: Men are slightly more likely to develop Parkinson’s disease than women.
- Oxidative Stress: Damage caused by free radicals in the brain is thought to contribute to the degeneration of dopamine-producing neurons.
Symptoms of Parkinson’s Disease
Parkinson’s disease is characterized by both motor and non-motor symptoms. These symptoms typically develop gradually and worsen over time.
Motor Symptoms
- Tremors: Involuntary shaking or trembling, often starting in one hand or arm. It is more noticeable at rest and can spread to other parts of the body.
- Bradykinesia: Slowness of movement, which can make simple tasks like buttoning a shirt or writing difficult.
- Rigidity: Stiffness and resistance to movement in the muscles, often leading to a stooped posture.
- Postural Instability: Difficulty maintaining balance, leading to a higher risk of falls.
- Freezing: Sudden, temporary inability to move, particularly when initiating a step or turning.
Non-Motor Symptoms
- Cognitive Changes: Memory problems, difficulty concentrating, and, in some cases, dementia.
- Mood Disorders: Depression, anxiety, and apathy are common in Parkinson’s disease.
- Sleep Disturbances: Insomnia, restless legs syndrome, and rapid eye movement (REM) sleep behavior disorder.
- Autonomic Dysfunction: Issues like constipation, urinary incontinence, and orthostatic hypotension (sudden drop in blood pressure when standing up).
- Speech and Swallowing Difficulties: Soft speech, monotone voice, and difficulty swallowing (dysphagia).
Diagnosis of Parkinson’s Disease
There is no specific test for Parkinson’s disease; diagnosis is based on clinical evaluation, medical history, and ruling out other conditions. The following tools and criteria are commonly used:
- Neurological Examination: Assessment of motor symptoms, such as tremors, bradykinesia, and rigidity.
- Unified Parkinson’s Disease Rating Scale (UPDRS): A scale used to evaluate the severity and progression of Parkinson’s symptoms.
- Levodopa Challenge Test: Improvement of symptoms after administering levodopa (a dopamine precursor) supports the diagnosis.
- Imaging: MRI or CT scans may be used to rule out other conditions, but they are not typically diagnostic for Parkinson’s disease.
Management of Parkinson’s Disease
While there is no cure for Parkinson’s disease, treatment focuses on managing symptoms and improving quality of life.
Pharmacologic Therapy
- Levodopa/Carbidopa (Sinemet):
- The most effective treatment for motor symptoms.
- Levodopa is converted to dopamine in the brain, while carbidopa prevents its breakdown before it reaches the brain.
- Dopamine Agonists:
- Medications like pramipexole and ropinirole mimic the effects of dopamine in the brain.
- Used in the early stages or in combination with levodopa.
- MAO-B Inhibitors:
- Medications like selegiline and rasagiline inhibit the breakdown of dopamine in the brain.
- COMT Inhibitors:
- Medications like entacapone are used with levodopa to prolong its effects.
- Amantadine:
- Provides mild symptomatic relief and helps manage levodopa-induced dyskinesias.
- Anticholinergics:
- Medications like benztropine are used to reduce tremors and rigidity, particularly in younger patients.
Surgical Options
- Deep Brain Stimulation (DBS):
- Involves implanting electrodes in specific areas of the brain to reduce motor symptoms.
- Typically used in patients who no longer respond well to medications.
- Pallidotomy or Thalamotomy:
- Surgical destruction of certain brain areas to alleviate symptoms, though less common than DBS.
Nursing Care for Parkinson’s Disease
Nursing care for patients with Parkinson’s disease focuses on promoting mobility, ensuring safety, managing medications, and providing emotional support.
Promoting Mobility and Preventing Falls
- Encourage Regular Exercise: Activities like walking, swimming, and stretching can help maintain muscle strength and flexibility.
- Assistive Devices: Use of canes, walkers, or handrails to aid in mobility and prevent falls.
- Modify the Environment: Remove trip hazards, provide adequate lighting, and use non-slip mats to reduce the risk of falls.
- Physical Therapy: Referral to a physical therapist for exercises to improve gait and balance.
Managing Medication
- Administer Medications on Time: Ensure that medications, especially levodopa, are given at consistent times to prevent fluctuations in symptoms.
- Monitor for Side Effects: Be aware of potential side effects of Parkinson’s medications, such as dyskinesias (involuntary movements), orthostatic hypotension, and hallucinations.
- Educate Patients and Families: Teach patients and caregivers about the importance of medication adherence and recognizing symptoms of “on-off” phenomena (fluctuations in response to levodopa).
Providing Emotional Support
- Address Mood Disorders: Be vigilant for signs of depression and anxiety, and provide appropriate referrals for mental health support.
- Encourage Social Interaction: Isolation can worsen symptoms; encourage participation in support groups or community activities.
- Support for Caregivers: Offer resources and respite care to alleviate caregiver burden.
Managing Non-Motor Symptoms
- Speech Therapy: Referral to a speech therapist for exercises to improve speech clarity and manage dysphagia.
- Nutritional Support: Ensure a well-balanced diet, and provide guidance on managing constipation and swallowing difficulties.
- Sleep Hygiene: Recommend good sleep practices, such as establishing a regular bedtime routine and avoiding caffeine before bedtime.
Sample NCLEX Questions
Question 1
A nurse is caring for a patient with Parkinson’s disease who is experiencing bradykinesia. Which of the following interventions should the nurse include in the plan of care?
A. Teach the patient to take large steps while walking.
B. Encourage the patient to perform ROM exercises every morning.
C. Provide a cane to assist with ambulation.
D. Remind the patient to avoid high-protein meals.
Answer: B. Encourage the patient to perform ROM exercises every morning.
Question 2
A patient with Parkinson’s disease is prescribed levodopa/carbidopa (Sinemet). Which side effect should the nurse monitor for?
A. Hyperglycemia
B. Orthostatic hypotension
C. Bradycardia
D. Insomnia
Answer: B. Orthostatic hypotension
Question 3
Which of the following symptoms is most indicative of early-stage Parkinson’s disease?
A. Dysphagia
B. Bradykinesia
C. Dementia
D. Postural instability
Answer: B. Bradykinesia
NCLEX Preparation Tips for Parkinson’s Disease
- Focus on Motor and Non-Motor Symptoms: Understand how Parkinson’s disease affects the body both physically and cognitively.
- Know the Medications: Be familiar with the common medications used to treat Parkinson’s and their side effects.
- Practice Nursing Interventions: Review care strategies for promoting mobility, ensuring safety, and managing medications.






