Understanding Dysrhythmias (Arrhythmias) for the NCLEX Exam
Dysrhythmias, also known as arrhythmias, are a key topic for the NCLEX exam and a critical aspect of cardiac nursing. These conditions involve abnormal heart rhythms that can affect the heart’s ability to pump blood effectively. This blog post will cover the types, causes, symptoms, diagnosis, treatment, and nursing interventions for dysrhythmias, along with sample NCLEX questions to enhance your exam preparation.
What are Dysrhythmias?
Dysrhythmias are disorders of the heart’s electrical system, resulting in irregular heartbeats. The heart may beat too fast (tachycardia), too slow (bradycardia), or irregularly, affecting the efficiency of blood circulation.
Types of Dysrhythmias
- Atrial Fibrillation (AFib): The most common type of dysrhythmia, where the atria quiver instead of contracting properly. This can lead to blood clots, stroke, and heart failure.
- Ventricular Tachycardia (VT): A rapid heart rate originating from the ventricles. It can be life-threatening if it leads to ventricular fibrillation.
- Ventricular Fibrillation (VFib): A severe, life-threatening dysrhythmia where the ventricles quiver instead of pumping blood effectively. Immediate defibrillation is required.
- Bradycardia: A slower than normal heart rate, usually defined as a heart rate below 60 beats per minute. It can be symptomatic, leading to dizziness, fatigue, and fainting.
- Supraventricular Tachycardia (SVT): A rapid heart rate that originates above the ventricles. It often starts and ends suddenly and can cause palpitations and shortness of breath.
- Premature Atrial Contractions (PACs): Early heartbeats originating from the atria. They are usually harmless but can be a sign of an underlying condition.
- Premature Ventricular Contractions (PVCs): Early heartbeats originating from the ventricles. Frequent PVCs may indicate an increased risk of more serious dysrhythmias.
Pathophysiology
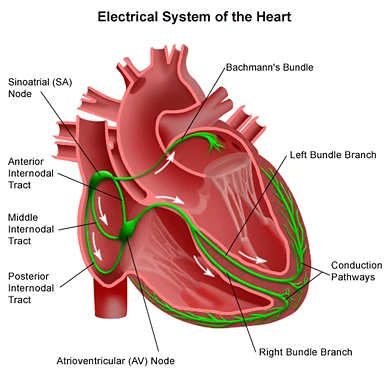
The heart’s electrical system controls the rhythm and rate of the heartbeat. Dysrhythmias occur when there is a disturbance in this electrical system, which can be due to:
- Abnormal Automaticity: The heart’s pacemaker cells (usually in the sinoatrial node) generate impulses irregularly.
- Re-entry Circuits: Electrical impulses re-enter and repeatedly stimulate the heart, leading to rapid heartbeats.
- Conduction Blocks: Impulses are delayed or blocked as they travel through the heart, leading to bradycardia or other rhythm disturbances.
- Ectopic Foci: Abnormal electrical impulses originate outside the normal pacemaker areas, leading to irregular rhythms.
Causes and Risk Factors
- Coronary Artery Disease (CAD): Narrowed or blocked arteries reduce blood flow to the heart, increasing the risk of dysrhythmias.
- Heart Failure: Weakened heart muscles can disrupt the electrical system.
- Electrolyte Imbalances: Abnormal levels of potassium, calcium, or magnesium can affect heart rhythm.
- Myocardial Infarction (Heart Attack): Damage to the heart muscle can lead to dysrhythmias.
- Medications: Certain drugs, such as beta-blockers, antiarrhythmics, and digoxin, can cause or exacerbate dysrhythmias.
- Stress: Emotional or physical stress can trigger dysrhythmias.
- Thyroid Disorders: Hyperthyroidism or hypothyroidism can affect heart rhythm.
- Sleep Apnea: Interrupted breathing during sleep can cause arrhythmias, particularly atrial fibrillation.
- Substance Use: Excessive alcohol, caffeine, or recreational drugs can induce dysrhythmias.
Symptoms
Symptoms of dysrhythmias can vary depending on the type and severity. Common symptoms include:
- Palpitations: Feeling like the heart is racing, pounding, or fluttering.
- Dizziness or Lightheadedness: Caused by a drop in blood pressure or decreased blood flow to the brain.
- Shortness of Breath: Especially during physical activity or when lying down.
- Fatigue: A result of the heart’s inability to pump blood efficiently.
- Chest Pain or Discomfort: Can occur if the heart isn’t getting enough oxygen.
- Syncope (Fainting): Caused by a sudden drop in blood pressure or heart rate.
Diagnosis
- Electrocardiogram (ECG or EKG): The primary tool for diagnosing dysrhythmias. It records the electrical activity of the heart and identifies abnormal rhythms.
- Holter Monitor: A portable ECG device worn for 24-48 hours to detect intermittent arrhythmias.
- Event Monitor: Similar to a Holter monitor, but worn for a longer period and activated by the patient when symptoms occur.
- Electrophysiological Study (EPS): A more invasive test that maps the electrical pathways of the heart and can induce arrhythmias for study.
- Echocardiogram: An ultrasound of the heart that assesses its structure and function.
- Stress Test: Assesses how the heart responds to physical exertion, which may trigger dysrhythmias.
Treatment
Medications
- Antiarrhythmics: Medications such as amiodarone, flecainide, or sotalol are used to control or prevent abnormal rhythms.
- Beta-Blockers: Slow the heart rate and reduce the force of contraction (e.g., metoprolol, propranolol).
- Calcium Channel Blockers: Help control heart rate, especially in atrial fibrillation (e.g., diltiazem, verapamil).
- Anticoagulants: Prevent blood clots in patients with atrial fibrillation (e.g., warfarin, apixaban).
Electrical Interventions
- Cardioversion: A procedure that uses electrical shocks to restore a normal heart rhythm, often used for atrial fibrillation or flutter.
- Pacemaker: A device implanted under the skin that regulates the heartbeat, especially in bradycardia.
- Implantable Cardioverter-Defibrillator (ICD): A device that monitors heart rhythm and delivers shocks if a dangerous rhythm is detected, often used in patients with a history of ventricular tachycardia or fibrillation.
- Catheter Ablation: A procedure that destroys small areas of heart tissue responsible for the abnormal rhythm, often used for supraventricular tachycardia or atrial fibrillation.
Lifestyle Modifications
- Dietary Changes: Reducing caffeine, alcohol, and high-fat foods can help manage symptoms.
- Stress Management: Techniques such as yoga, meditation, and regular exercise can reduce stress-induced dysrhythmias.
- Smoking Cessation: Quitting smoking can improve heart health and reduce arrhythmia risk.
- Weight Management: Maintaining a healthy weight helps reduce the strain on the heart.
Nursing Interventions
- Monitor Vital Signs: Regularly check heart rate, rhythm, and blood pressure.
- Administer Medications: Ensure correct dosage and timing of antiarrhythmics, beta-blockers, or anticoagulants.
- Patient Education: Teach patients about their condition, medication adherence, and lifestyle changes.
- Prepare for Procedures: Assist in the preparation and recovery of patients undergoing cardioversion, pacemaker insertion, or ablation.
- Recognize and Report: Be alert for signs of complications, such as worsening symptoms, signs of stroke, or adverse reactions to medications.
Sample NCLEX Questions
Question 1
A patient with atrial fibrillation is at risk for which of the following complications?
A. Myocardial infarction
B. Pulmonary embolism
C. Stroke
D. Deep vein thrombosis
Answer: C. Stroke
Question 2
A nurse is administering digoxin to a patient with atrial fibrillation. What is the most important parameter to assess before giving the medication?
A. Blood pressure
B. Respiratory rate
C. Heart rate
D. Oxygen saturation
Answer: C. Heart rate
Question 3
A patient with ventricular tachycardia is unresponsive and pulseless. What is the priority nursing action?
A. Administer epinephrine
B. Perform defibrillation
C. Start chest compressions
D. Prepare for cardioversion
Answer: B. Perform defibrillation
Question 4
Which of the following is a potential side effect of amiodarone, an antiarrhythmic medication?
A. Hyperkalemia
B. Hypothyroidism
C. Tachycardia
D. Thrombocytopenia
Answer: B. Hypothyroidism
NCLEX Preparation Tips for Dysrhythmias
- Understand ECG Readings: Be familiar with how to interpret common dysrhythmias on an ECG.
- Know the Symptoms: Recognize the signs and symptoms of different dysrhythmias.
- Medication Knowledge: Understand the mechanisms, uses, and side effects of medications used to treat dysrhythmias.
- Emergency Protocols: Know the steps for managing life-threatening dysrhythmias, such as ventricular fibrillation.
- Practice Questions: Use NCLEX-style questions to test your knowledge and application of dysrhythmia concepts.






