Understanding Vascular Disease: A Comprehensive Guide for Nurses
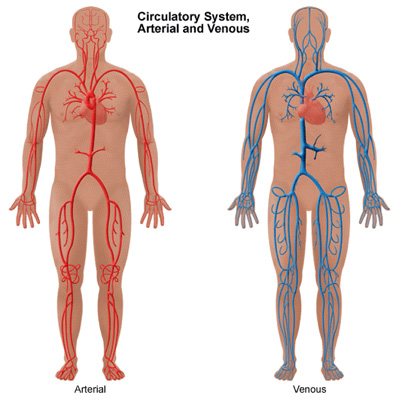
Vascular disease encompasses a range of conditions that affect the blood vessels, including arteries, veins, and capillaries. It can lead to significant health complications if not managed properly. This guide provides an overview of vascular disease, common symptoms, treatment options, and nursing care considerations, adhering to NCLEX standards.
What is Vascular Disease?
Vascular disease refers to any condition that affects the circulatory system. The most common types include:
- Atherosclerosis: Hardening and narrowing of the arteries due to plaque buildup.
- Peripheral Artery Disease (PAD): Reduced blood flow to the limbs, usually the legs, due to narrowed arteries.
- Aneurysm: An abnormal bulge in the wall of a blood vessel.
- Varicose Veins: Swollen, twisted veins usually occurring in the legs.
- Deep Vein Thrombosis (DVT): Formation of a blood clot in a deep vein, typically in the legs.
Common Symptoms of Vascular Disease
The symptoms of vascular disease vary depending on the type and severity. Common symptoms include:
- Atherosclerosis and PAD:
- Leg pain when walking (claudication)
- Numbness or weakness in the legs
- Coldness in the lower leg or foot
- Sores on the toes, feet, or legs that won’t heal
- Aneurysm:
- Pain in the area of the aneurysm
- Pulsating feeling near the navel (abdominal aortic aneurysm)
- Varicose Veins:
- Visible, twisted veins
- Aching pain and discomfort
- Swelling in the lower legs
- DVT:
- Swelling in one leg
- Pain or tenderness in the leg
- Warmth in the affected leg
Diagnosis and Treatment
Diagnosis
Diagnosis of vascular disease typically involves:
- Physical Examination: Checking for signs like weak or absent pulses in the legs.
- Imaging Tests: Including ultrasound, CT scans, MRI, and angiography.
- Blood Tests: To check for markers of inflammation and other conditions.
Treatment
Treatment varies based on the specific condition but may include:
- Lifestyle Changes: Including quitting smoking, exercising, and eating a healthy diet.
- Medications: To manage symptoms and prevent complications, such as anticoagulants for DVT or statins for atherosclerosis.
- Surgical Interventions: Procedures like angioplasty, bypass surgery, or vein stripping.
Nursing Care and Considerations
Nurses play a crucial role in the management and care of patients with vascular disease. The following are key nursing considerations and interventions:
1. Assessment
- Thorough History: Obtain a detailed health history, including risk factors such as smoking, diabetes, hypertension, and family history of vascular disease.
- Physical Assessment: Regularly monitor vital signs, peripheral pulses, skin temperature, and color of extremities.
2. Patient Education
- Lifestyle Modifications: Educate patients on the importance of quitting smoking, adhering to a healthy diet, and engaging in regular physical activity.
- Medication Adherence: Ensure patients understand their medication regimen, including the purpose, dosage, and potential side effects.
- Signs and Symptoms: Teach patients to recognize symptoms of complications, such as signs of a stroke, heart attack, or worsening PAD.
3. Preventive Measures
- DVT Prophylaxis: Implement measures to prevent DVT in at-risk patients, such as encouraging ambulation, using compression stockings, and administering anticoagulants as prescribed.
- Skin Care: Educate patients with varicose veins or PAD on proper skin care to prevent ulcers and infections.
4. Monitoring and Follow-up
- Regular Monitoring: Continuously assess the patient’s condition, monitor for any changes, and report significant findings to the healthcare provider.
- Follow-up Appointments: Encourage patients to keep all follow-up appointments for ongoing evaluation and management.
Case Study: Managing a Client with Peripheral Artery Disease (PAD)
Background
Mr. Smith, a 65-year-old man with a history of smoking and diabetes, presents with complaints of leg pain while walking and sores on his toes that are slow to heal.
Assessment
- History: Long-term smoker, poorly controlled diabetes, family history of cardiovascular disease.
- Physical Exam: Weak pulses in the lower extremities, cool skin temperature, non-healing sores on the toes.
Diagnosis
Mr. Smith is diagnosed with Peripheral Artery Disease (PAD) based on his symptoms and diagnostic tests, including an ankle-brachial index (ABI) test.
Treatment Plan
- Lifestyle Modifications: Smoking cessation program, dietary changes to manage diabetes, and a supervised exercise program.
- Medications: Prescribed antiplatelet agents and statins to manage cholesterol levels.
- Wound Care: Proper wound care for the sores on his toes to prevent infection.
- Education: Educated on the importance of foot care, monitoring blood glucose levels, and adhering to the treatment plan.
Nursing Interventions
- Monitoring: Regularly monitor peripheral pulses, skin condition, and signs of infection.
- Patient Education: Reinforce the importance of lifestyle changes, medication adherence, and follow-up care.
- Support: Provide emotional support and resources for smoking cessation and diabetes management.
Conclusion
Vascular disease requires comprehensive care and management to prevent complications and improve quality of life. Nurses play a pivotal role in assessing, educating, and supporting patients with vascular disease. By following evidence-based practices and providing holistic care, nurses can significantly impact patient outcomes.
If you or someone you know is experiencing symptoms of vascular disease, seek medical advice promptly for proper diagnosis and treatment.






