Mastering Peptic Ulcer Disease (PUD) for the NCLEX Exam
Peptic ulcer disease (PUD) is a common gastrointestinal condition that you may encounter in clinical practice, making it an important topic for the NCLEX exam. This blog post will cover the essential aspects of PUD, including its pathophysiology, symptoms, diagnosis, treatment, and nursing interventions. We’ll also include practice questions to help you prepare effectively for the exam.
What is Peptic Ulcer Disease (PUD)?
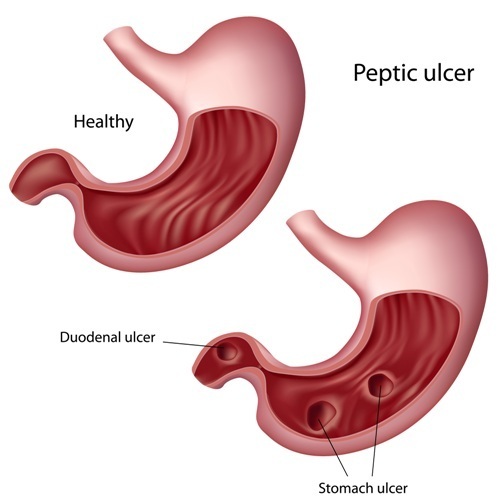
Peptic ulcer disease (PUD) refers to the formation of open sores, or ulcers, in the lining of the stomach, duodenum, or esophagus. These ulcers occur when the protective mucosal lining is compromised, allowing gastric acid to erode the tissue. The two most common types of PUD are:
- Gastric Ulcers: Occur in the stomach lining.
- Duodenal Ulcers: Occur in the duodenum, the first part of the small intestine.
Pathophysiology
Peptic ulcers develop due to an imbalance between the digestive fluids in the stomach and duodenum. This imbalance can be caused by several factors:
- Helicobacter pylori (H. pylori) Infection: A bacterium that weakens the protective mucous coating of the stomach and duodenum, leading to ulcer formation.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications can disrupt the mucosal lining by inhibiting prostaglandin production, which normally protects the stomach lining.
- Excessive Acid Production: Conditions like Zollinger-Ellison syndrome can cause an overproduction of gastric acid, leading to ulcers.
- Smoking and Alcohol Use: Both can increase gastric acid production and irritate the stomach lining.
- Stress: While stress itself doesn’t cause ulcers, it can exacerbate symptoms in those who already have PUD.
Symptoms
- Epigastric Pain: A burning or gnawing pain in the upper abdomen, often occurring between meals or at night.
- Bloating and Belching: Due to gas buildup in the stomach.
- Nausea and Vomiting: May occur with or without blood (hematemesis).
- Weight Loss: Unintended weight loss due to decreased appetite and food avoidance.
- Melena: Black, tarry stools indicating gastrointestinal bleeding.
Risk Factors
- H. pylori Infection
- Chronic NSAID Use
- Smoking
- Excessive Alcohol Consumption
- Advanced Age
- History of Ulcers
- Family History of PUD
- High-Stress Lifestyle
Diagnosis
- Endoscopy: The gold standard for diagnosing PUD. It allows direct visualization of the ulcers and biopsy for H. pylori testing.
- H. pylori Testing: Can be done via urea breath test, stool antigen test, or biopsy during endoscopy.
- Upper GI Series (Barium Swallow): An X-ray examination of the upper digestive tract.
- Blood Tests: To check for anemia or other signs of bleeding.
Treatment
Pharmacological Management
- Proton Pump Inhibitors (PPIs): Drugs like omeprazole, esomeprazole, and pantoprazole reduce stomach acid production and promote ulcer healing.
- H2-Receptor Antagonists: Medications such as ranitidine and famotidine decrease acid production.
- Antibiotics: To eradicate H. pylori infection, typically in combination with PPIs.
- Antacids: Provide symptomatic relief by neutralizing stomach acid.
- Cytoprotective Agents: Drugs like sucralfate coat the ulcer and protect it from acid.
Lifestyle Modifications
- Avoid NSAIDs: Substitute with acetaminophen or other alternatives.
- Limit Alcohol and Smoking: Both exacerbate ulcer formation and delay healing.
- Dietary Adjustments: Avoid foods that irritate the stomach, such as spicy, acidic, or fatty foods.
- Stress Management: Implementing stress-reduction techniques like meditation or yoga.
Complications
- Perforation: A hole in the stomach or duodenum, leading to peritonitis.
- Gastrointestinal Bleeding: Can result in hematemesis or melena and may require emergency treatment.
- Gastric Outlet Obstruction: Due to swelling or scarring, blocking the passage of food.
- Anemia: Chronic blood loss from the ulcer can lead to iron-deficiency anemia.
Nursing Interventions
- Monitor Vital Signs: Especially if there is evidence of bleeding or shock.
- Assess Pain: Regularly evaluate pain and administer analgesics as prescribed.
- Administer Medications: Ensure compliance with PPIs, H2-receptor antagonists, and antibiotics.
- Educate the Patient: Discuss the importance of medication adherence, lifestyle changes, and follow-up care.
- Monitor for Complications: Be vigilant for signs of perforation, bleeding, or obstruction.
- Dietary Counseling: Provide guidance on a bland diet, avoiding irritants, and small, frequent meals.
Sample NCLEX Questions
Question 1
A patient with a history of peptic ulcer disease presents to the emergency department with severe epigastric pain, a rigid abdomen, and absent bowel sounds. Which of the following complications should the nurse suspect?
A. Gastrointestinal bleeding
B. Perforation
C. Gastric outlet obstruction
D. Chronic gastritis
Answer: B. Perforation
Question 2
A nurse is providing discharge teaching to a patient with peptic ulcer disease. Which statement by the patient indicates a need for further education?
A. “I will avoid taking ibuprofen and use acetaminophen for pain relief.”
B. “I should take my omeprazole every morning before breakfast.”
C. “I will stop drinking alcohol to help prevent another ulcer.”
D. “I can continue smoking as long as I limit it to one pack a day.”
Answer: D. “I can continue smoking as long as I limit it to one pack a day.”
Question 3
A patient with peptic ulcer disease is prescribed a combination therapy including omeprazole, clarithromycin, and amoxicillin. What is the primary goal of this therapy?
A. To reduce stomach acid production
B. To eradicate H. pylori infection
C. To relieve pain and discomfort
D. To prevent complications of PUD
Answer: B. To eradicate H. pylori infection
Question 4
Which of the following dietary recommendations should the nurse include in the care plan for a patient with peptic ulcer disease?
A. Consume three large meals per day
B. Avoid caffeine, alcohol, and spicy foods
C. Increase intake of citrus fruits and juices
D. Limit fluid intake to avoid overhydration
Answer: B. Avoid caffeine, alcohol, and spicy foods
NCLEX Preparation Tips for Peptic Ulcer Disease
- Understand the Pathophysiology: Be clear on how PUD develops and the role of H. pylori and NSAIDs.
- Recognize Symptoms: Know the classic symptoms and how to distinguish between gastric and duodenal ulcers.
- Diagnostic Tests: Familiarize yourself with the diagnostic tools used for PUD.
- Treatment Protocols: Understand the medications used in PUD management and their specific purposes.
- Complication Awareness: Be aware of potential complications and their clinical manifestations.
- Practice Questions: Use NCLEX-style questions to reinforce your knowledge and improve your exam readiness.
Conclusion
Peptic ulcer disease is a key topic for the NCLEX exam, requiring a solid understanding of its causes, symptoms, treatment, and potential complications. By mastering this content and practicing related NCLEX questions, you will be well-prepared to answer PUD questions on the exam and provide effective care to patients with this condition. Keep studying, practicing, and applying your knowledge to excel in your nursing career.






